What is CBT?
In CBT, the client is the expert in themselves and in what they need to effect change in their life. The client has borne witness to their lived experience and, as such, is best placed to identify, in collaboration with the therapist, what they believe, what they think, how they feel this or interpret these thoughts, and what effect this has on their lives.
We are all capable of both rational and irrational thoughts.
Rational thinking considers a situation with the ability to organize and analyze relevant information to come to a sound conclusion, one which helps the person positively use the result in their life.
Irrational thinking is where the client takes information and can often involve making faulty decisions or coming to a conclusion, which may be partially or entirely incorrect due to the influence of preconceptions on their thinking process.
For example, let's take a situation when a person is about to leave the house, and it begins to rain. A rational thought may be, “I’ll put on a coat, and I’ll be fine.” An irrational thought may be, “I’ll get soaked ...... and I’ll get sick and die.”
The Cognitive Model
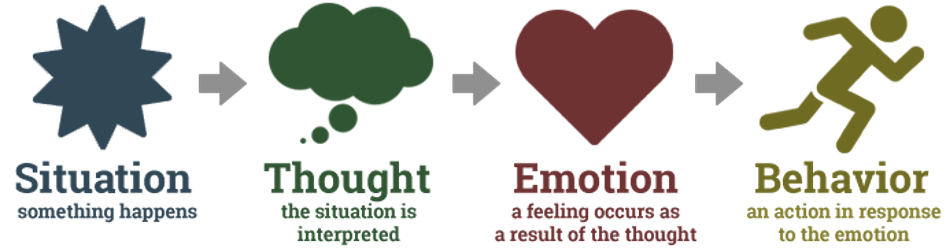
In CBT, the theory is that thoughts lead to behaviours. That is, a thought will create a feeling in the person, an emotional reaction, which then leads to the person behaving in a certain way, taking action in response to the emotional reaction to the thought.
In the previous example where the person is about to leave the house, and it begins to rain (the situation), the person having a positive emotional reaction (the emotion) after sizing up the situation (the thought) may simply put on a coat going out and get on with their day’s business (the behaviour).
On the other hand, the person having the irrational thought where they picture themselves getting sick and dying may retreat into the house, afraid to go out, and not get to do whatever they were leaving to do. This, in turn, may have the effect of causing other problems in their life which could then lead to more stress and anxiety.
So, CBT aims to teach this second person to arrest this process at the point where they have the thought which creates the emotional reaction. The CBT therapist will work with the client to help them to understand how they think and how that links with the behaviour that’s causing a problem in their life.
The aim is to give this client the tools they need to identify and change their unhelpful behavioural patterns by making adjustments to their thinking styles. These adjustments to the client’s thinking patterns will help to alleviate their distress in the here and now, as well as to give them the tools to do so in the future when similar patterns emerge for them.
CBT can also be used to help a client identify and challenge core beliefs which may be holding them back and causing distress in their life.
The Role of the Therapist In CBT
So where does the therapist come into this? The therapist role is as a collaborator with the client in the process of identifying irrational thinking and in the process of developing and implementing plans to help the client arrest and rationally analyze these thoughts.
The therapist explains the CBT process to the client, so they know what to expect and how to work within it.
Then they both collaborate in identifying areas of concern to the client and in formulating plans and solutions to help alleviate the client’s distress.
CBT Sessions:
The number of sessions for CBT varies and depends on the needs of the individual. For short CBT, the number of sessions can be approximately 10-12, with each session being around 50-60 minutes. The therapeutic process may consist of one session per week, or therapists may schedule more frequent sessions, depending on your needs.
A standard CBT session involves setting an agenda at the start. It focuses on important, prioritized targets. The therapeutic process then follows that agenda, but it is also flexible should an unplanned and critical topic emerges. CBT is a collaborative approach. The therapist will work with you to identify your needs, and they plan treatment accordingly.
To meet these goals, the therapist uses different CBT techniques. These techniques are cognitive restructuring, systematic desensitization, meditation, exposure techniques, and others. Another important aspect of CBT is homework or exercises to practice outside of therapy.
Practice at Home
Practicing at home will be a vital element of any CBT treatment plan and demands a commitment from the client to continue, outside of sessions, the work being done in the therapist’s room. It is a crucial element of CBT, and it is planned collaboratively between the client and the therapist to practice new skills and coping strategies as well as to restructure maladaptive beliefs.
Effectiveness of CBT
As it is arguably the most studied form of psychotherapy, there is a very robust evidence base for CBT as a psychotherapeutic treatment, especially with regards to anxiety and depression with CBT often referred to as “the gold standard treatment”.
CBT has been found to be effective in the treatment of Anxiety, Depression, PTSD, Phobias, Seasonal Affective Disorder (SAD), Post Traumatic Stress Disorder (PTSD), Obsessive-Compulsive Disorder (OCD), sleep issues and is also highly effective in emotional regulation and addiction relapse prevention.
Advantages of CBT
CBT has many benefits or advantages over other forms of treatment.
For example, CBT can be as useful, and sometimes more useful, in treating some disorders than medication, and can also work in conjunction with medication. It will often entail a much shorter term of treatment, requiring fewer sessions, than other forms of treatment, such as applying psychodynamic theory.
CBT is also highly adaptable and can take different formats, depending on the client’s presenting issues. As a collaborative effort between the therapist and the client, the client is empowered by their involvement in designing their treatment plans and solutions, as well as in gaining skills which can be applied throughout their life.
CBT can be useful for any age group.